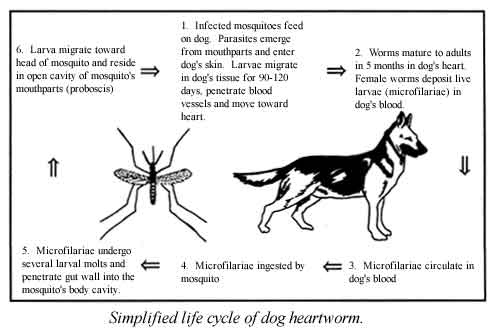
- Obligatory vectors. Obligatory vectors of disease include those in which the pathogen develops from one life-cycle stage to another. Malaria is an example of a disease that must be taken up by a vector (mosquito) to develop from one stage to another. Otherwise, the malaria parasite would die. Mosquitoes are often obligatory vectors of diseases.
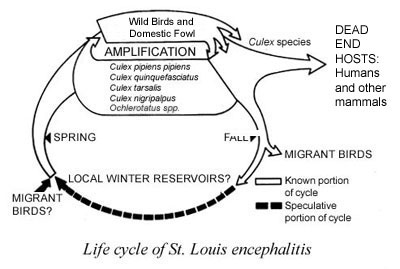
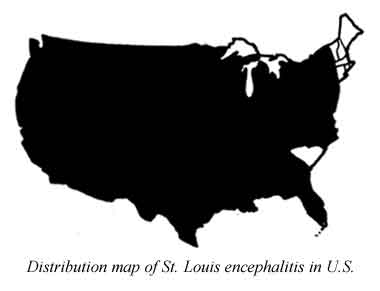
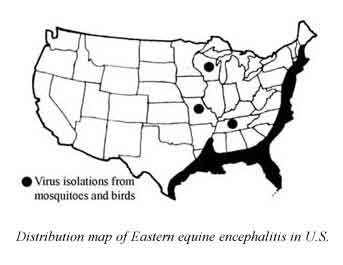
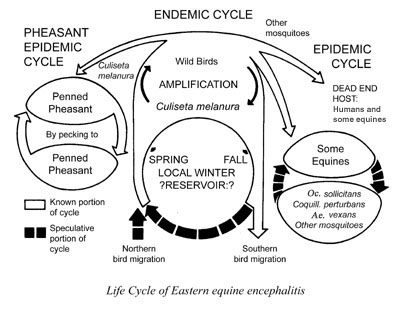
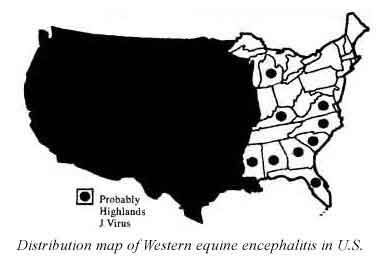
- Reservoir hosts. Reservoirs are defined as one or more host species that harbor a disease-causing pathogen over an extended period of time without showing symptoms of the disease. Disease transmission can occur when a vector feeds on a host that carries the pathogen then feeds on another, susceptible host. Birds are an example of reservoirs for mosquito-borne encephalitis, which can affect humans, horses or other dead-end hosts — those from which susceptible mosquitoes cannot acquire an infection. In many cases the disease is endemic, that is, it exists continually in reservoirs in a geographically defined area. Diseases that cycle in nature to nonreservoir hosts without involving humans are called zoonoses. When a disease outbreak occurs in these nonhuman animals, it is called an epizootic.
- Transovarial transmission. Some vectors pass the disease to their offspring through eggs. When the female is infected with the disease organism, her eggs become infected and the resulting larvae are infected with the disease. The subsequent adult stage is then infected and can transmit the pathogen without needing to feed on an infected host. This occurs with several mosquito-borne viruses and with Rickettsia rickettsia causing Rocky Mountain spotted fever. In that instance the tick and the mosquito serve both as reservoir and vector.
Modes of biological transmission:
II. POISON IRRITATION AND ALLERGY
 |
 |
 |
 |
IV. IMAGINARY PEST INFESTATIONS
University of Florida and the American Mosquito Control Association
Public Health Pest Control WWW site at http://entomology.ifas.ufl.edu/fasulo/vector/
Additional Resources:
- CDC - Dengue Fever/Dengue Hemorrhagic Fever
- CDC - Domestic Arboviral Encephalitides
- CDC - Plague
- CDC - Updated information regarding Insect Repellents
- CDC - West Nile Virus
- CDC - Yellow Fever
- NBII - West Nile Virus
- UF/IFAS - Chikungunya
- UF/IFAS - La Fiebre Chikungunya
- UF/IFAS - What is Dengue?
- UF/IFAS - Leishmaniasis
- UF/IFAS - La Leishmaniosis
- UF/IFAS - Yellow Fever
- UF/IFAS - La Fiebre Amarilla
- UF/IFAS - Florida Medical Entomology Laboratory
Return to Public Health Pest Control Menu
http://entomology.ifas.ufl.edu/fasulo/vector/